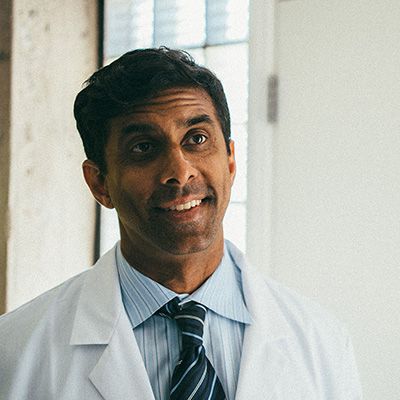
Grow a mo
Growing a Mo is like wearing a symbol representing healthier men and a healthier world, all Movember long. It shows everyone you walk past that men’s health matters to you.
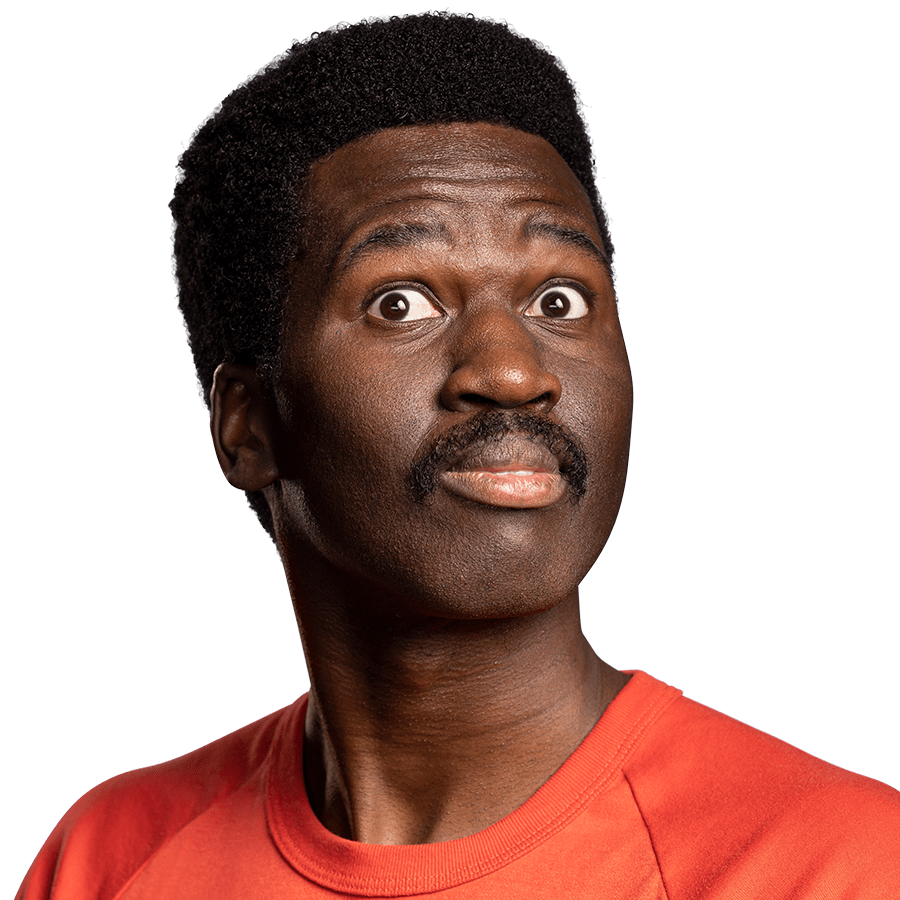
Move for Mental Health
Move is how The Order of Mo remembers the 60 men suicide takes globally, every hour. To take part, all you have to do is run or walk 60 miles over Movember.

Host a Mo-ment
Make having a good time your goal and you won’t go wrong. Get your believers, supporters and followers around. Host an event that raises awareness and funds for men’s health.

Mo your own way
There are many ways to better men’s health. And if you believe doing your own thing is it, we're 100% getting behind you.

Movember fundraisers are a global community of fired up Mo Bros and Mo Sisters – aka rock stars making a difference in mental health and suicide prevention, prostate cancer and testicular cancer.
Your donation could help save a father, a brother, a son, a friend, a partner, a man’s life.